How to Know if You Have a Damaged Rotator Cuff
Signs & Symptoms | Mechanisms of Injury | Diagnosis | Prevention | Handling | Conservative | Surgery | Rehabilitation
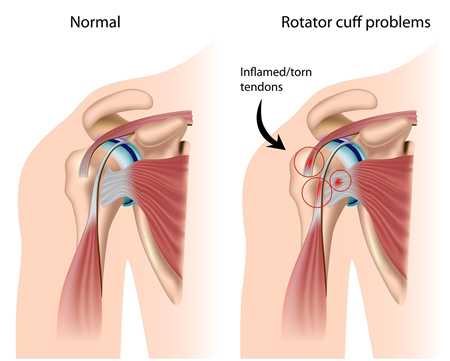 A rotator cuff tear is a tear of ane or more of the tendons of the four rotator cuff muscles of the shoulder. A rotator cuff 'injury' can include whatsoever type of irritation or overuse of those muscles or tendons, and is among the most common atmospheric condition affecting the shoulder.
A rotator cuff tear is a tear of ane or more of the tendons of the four rotator cuff muscles of the shoulder. A rotator cuff 'injury' can include whatsoever type of irritation or overuse of those muscles or tendons, and is among the most common atmospheric condition affecting the shoulder.
The tendons of the rotator cuff, not the muscles, are most commonly involved, and of the four, the supraspinatus is most frequently afflicted, as it passes below the acromion. Such a tear ordinarily occurs at its bespeak of insertion onto the humeral head at the greater tubercle.
The cuff is responsible for stabilizing the glenohumeral joint, abducting, externally rotating, and internally rotating the humerus. When shoulder trauma occurs, these functions can be compromised. Because individuals are highly dependent on the shoulder for many activities, overuse of the muscles can atomic number 82 to tears, the vast majority again occurring in the supraspinatus tendon.
Signs and Symptoms
Many rotator gage tears are asymptomatic. They are known to increase in frequency with age and the most common crusade is age-related degeneration and, less oft, sports injuries or trauma. Both partial and full thickness tears take been institute on post mortem and MRI studies in those without whatsoever history of shoulder pain or symptoms. However, the virtually common presentation is shoulder pain or discomfort. This may occur with activeness, especially shoulder activity above the horizontal position, but may also be nowadays at balance in bed. Hurting-restricted move in a higher place the horizontal position may be present, besides as weakness with shoulder flexion and abduction.
Mechanisms of injury
The ii main causes are injury (acute) and degeneration (chronic and cumulative), and the mechanisms involved can be either extrinsic or intrinsic or, probably virtually normally, a combination of both.
Acute tears
The amount of stress needed to tear a rotator gage tendon acutely volition depend on the underlying status of the tendon prior to the stress. In the case of a healthy tendon, the stress needed will be high, such as a fall on the outstretched arm. This stress may occur coincidentally with other injuries such as a dislocation of the shoulder, or separation of the acromioclavicular joint. In the case of a tendon with pre-existing degeneration, the strength may be surprisingly modest, such as a sudden lift, especially with the arm higher up the horizontal position. This is a common occurrence with rear seated passengers in a motor vehicle collision, regardless of speed.
Chronic tears
Chronic tears are indicative of extended use in conjunction with other factors such equally poor biomechanics or muscular imbalance. Ultimately, well-nigh are the result of vesture that occurs slowly over time as a natural part of crumbling. They are more mutual in the dominant arm, but a tear in i shoulder signals an increased risk of a tear in the opposing shoulder. Several factors contribute to degenerative, or chronic, rotator cuff tears of which repetitive stress is the most significant. This stress consists of repeating the aforementioned shoulder motions oftentimes, such every bit overhead throwing, rowing, and weightlifting. Many jobs that require frequent shoulder movement such as lifting and overhead movements as well contribute.
Another factor in older populations is impairment of blood supply. With age, apportionment to the rotator cuff tendons decreases, impairing natural power to repair, ultimately leading to, or contributing to, tears.
The final common gene is impingement syndrome, the most common nonsports-related injury and which occurs when the tendons of the rotator cuff muscles become irritated and inflamed while passing through the subacromial space below the acromion. This relatively small space becomes even smaller when the arm is raised in a forrad or upward position. Repetitive impingement can inflame the tendons and bursa, resulting in the syndrome.
Extrinsic factors
Well-documented anatomical factors include the morphologic characteristics of the acromion. Hooked, curved, and laterally sloping acromia are strongly associated with cuff tears and may cause tractional damage to the tendon.[10] Conversely, apartment acromia may have an insignificant involvement in gage illness and consequently may exist best treated conservatively. The evolution of these different acromial shapes is probable both genetic and acquired. In the latter case, only historic period has been positively correlated with progression from flat to curved or hooked. The nature of mechanical activities, such every bit sports involving the shoulder, along with frequency and intensity of such sports, may be responsible for the adverse development. Sports such equally bowling in cricket, pond, lawn tennis, baseball, and kayaking, are nearly often implicated. However, a progression to a hooked acromion may simply be an adaptation to an already damaged, poorly counterbalanced rotator gage that is creating increasing stress on the coracoacromial curvation. Other anatomical factors that may have significance include os acromiale and acromial spurs. Environmental factors implicated include increasing age, shoulder overuse, smoking, and any medical condition that affects circulation or impairs the inflammatory and healing response, such as diabetes mellitus.
Intrinsic factors
Intrinsic factors refer to injury mechanisms that occur within the rotator cuff itself. The main is a degenerative-microtrauma model, which supposes that historic period-related tendon impairment compounded by chronic microtrauma results in partial tendon tears that then develop into full rotator cuff tears. Every bit a result of repetitive microtrauma in the setting of a degenerative rotator cuff tendon, inflammatory mediators alter the local environs, and oxidative stress induces tenocyte apoptosis causing farther rotator cuff tendon degeneration. A neural theory also exists that suggests neural overstimulation leads to the recruitment of inflammatory cells and may also contribute to tendon degeneration.
Diagnosis
Diagnosis is based upon physical assessment and history, including clarification of previous activities and acute or chronic symptoms. A systematic, concrete exam of the shoulder comprises inspection, palpation, range of motion, provocative tests to reproduce the symptoms, neurological exam, and forcefulness testing.The shoulder should besides be examined for tenderness and deformity. Since pain arising from the neck is oft 'referred' to the shoulder, the examination should include an assessment of the cervical spine looking for evidence suggestive of a pinched nerve, osteoarthritis, or rheumatoid arthritis.
Diagnostic modalities, dependent on circumstances, include X-ray, MRI, MR arthrography, double-contrast arthrography, and ultrasound. Although MR arthrography is currently considered the gilded standard, ultrasound may be about toll-effective. Ordinarily, a tear will exist undetected by X-ray, although os spurs, which can impinge upon the rotator cuff tendons, may be visible. Such spurs suggest chronic severe rotator gage disease. Double-contrast arthrography involves injecting contrast dye into the shoulder joint to observe leakage out of the injured rotator cuff and its value is influenced by the feel of the operator. The well-nigh common diagnostic tool is magnetic resonance imaging (MRI), which tin can sometimes bespeak the size of the tear, also as its location within the tendon. Furthermore, MRI enables the detection or exclusion of complete rotator gage tears with reasonable accurateness and is likewise suitable to diagnose other pathologies of the shoulder joint.
The logical use of diagnostic tests is an important component of effective clinical do. X-rays cannot directly reveal tears of the rotator gage, a 'soft tissue', and consequently, normal X-rays cannot exclude a damaged cuff. However, indirect evidence of pathology may be seen in instances where one or more than of the tendons have undergone degenerative calcification (calcific tendinitis). Also, large tears of the rotator cuff may permit the humeral head to migrate upwards (high-riding humeral caput) which may be visible on 10-ray. Prolonged contact between a high-riding humeral head and the acromion above it, may lead to X-rays findings of wear on the humeral head and acromion and secondary degenerative arthritis of the glenohumeral articulation (the ball and socket joint of the shoulder), called cuff arthropathy, may follow. Incidental X-ray findings of bone spurs at the adjacent acromioclavicular articulation may show a os spur growing from the outer edge of the clavicle downwards towards the rotator cuff. Spurs may also be seen on the underside of the acromion, in one case thought to cause direct fraying of the rotator cuff from contact friction, a concept currently regarded as controversial.
Clinical judgement, rather than over reliance on MRI or any other modality, is strongly brash in determining the cause of shoulder pain, or planning its handling, since rotator gage tears are also found in some without pain or symptoms. The role of X-ray, MRI, and ultrasound, is adjunctive to clinical cess and serves to confirm a diagnosis provisionally fabricated by a thorough history and physical exam. Over-reliance on imaging may potentially atomic number 82 to overtreatment or lark from the true underlying problem.
Prevention
Long-term overuse/abuse of the shoulder joint is mostly thought to limit range of motion and productivity due to daily clothing and tear of the muscles, and many public web sites offer preventive advice. The recommendations usually include:
- regular shoulder exercises to maintain strength and flexibility
- using proper grade when lifting or moving heavy weights
- resting the shoulder when experiencing pain
- application of cold packs and heat pads to a painful, inflamed shoulder
- strengthening program to include the back and shoulder girdle muscles likewise as the chest, shoulder and upper arm
- adequate rest periods in occupations that require repetitive lifting and reaching
Size
According to a report which measured tendon length against the size of the injured rotator cuff, researchers learned that as rotator cuff tendons decrease in length, the average rotator cuff severity is proportionally decreased, too. This shows that larger individuals are more likely to suffer from a severe rotator cuff tear if they do not tighten the shoulder muscles around the articulation.
Position
Another study observed 12 different positions of movements and their relative correlation with injuries occurred during those movements. The evidence shows that putting the arm in a neutral position relieves tension on all ligaments and tendons.
Stretching
One article observed the influence of stretching techniques on preventative methods of shoulder injuries. Increased velocity of practise increases injury, but showtime a fast-movement exercise with a slow stretch may crusade muscle/tendon zipper to become more resistant to tearing.
Muscle groups
When exercising, exercising the shoulder as a whole and non one or two muscle groups is also constitute to be imperative. When the shoulder muscle is exercised in all directions, such as external rotation, flexion, and extension, or vertical abduction, it is less likely to suffer from a tear of the tendon.
Handling
Those suspected of having a rotator cuff tear are potentially candidates for either operative or not-operative (bourgeois) handling. Notwithstanding, whatever individual may move from one grouping to the other based on clinical response and findings on repeated exam.
No testify of benefit is seen from early rather than delayed surgery, and many with partial tears and some with complete tears will respond to non-operative management. Consequently, many recommend initial, nonsurgical management. Yet, early surgical treatment may be considered in significant (>1 cm-1.5 cm) astute tears or in young patients with full-thickness tears who have a significant risk for the development of irreparable rotator cuff changes.
Conservative
Those with pain but reasonably maintained office are suitable for nonoperative management. This includes oral medications that provide hurting relief such as anti-inflammatory agents, topical pain relievers such as cold packs, and if warranted, subacromial corticosteroid/local anesthetic injection. A sling may be offered for short-term condolement, with the understanding that undesirable shoulder stiffness can develop with prolonged immobilization. Early physical therapy may afford hurting relief with modalities (e.yard. iontophoresis) and help to maintain move. Ultrasound treatment is not efficacious. As pain decreases, strength deficiencies and biomechanical errors can be corrected.
A conservative physical therapy program begins with preliminary rest and brake from engaging in activities which gave rise to symptoms. Normally, inflammation can ordinarily be controlled within i to 2 weeks, using a nonsteroidal anti-inflammatory drug and subacromial steroid injections to decrease inflammation, to the point that pain has been significantly decreased to make stretching tolerable. After this short period, rapid stiffening and an increment in pain can consequence if sufficient stretching has non been implemented.
A gentle, passive range-of-motility program should exist started to aid prevent stiffness and maintain range of motility during this resting period. Exercises, for the anterior, inferior, and posterior shoulder, should be part of this program. The employ of NSAIDs, hot and cold packs, and physical therapy modalities, such equally ultrasound, phonophoresis, or iontophoresis, can exist instituted during this stretching menstruation, if effective. Corticosteroid injections are recommended two to three months apart with a maximum of 3 injections. Multiple injections (four or more) have been shown to compromise the results of rotator cuff surgery which result in weakening of the tendon. Withal, before whatsoever rotator gage strengthening can be started, the shoulder must have a total range of movement.
After a full, painless range of motion is achieved, the patient may advance to a gentle strengthening plan. This plan is aimed at creating an do regimen that initially gently improves motion, then gradually improves forcefulness in the shoulder girdle.
Several instances occur in which nonoperative treatment would non be suggested:
- 20 to 30-year-erstwhile agile patient with an acute tear and severe functional deficit from a specific event
- 30 to 50-year-quondam patient with an astute rotator cuff tear secondary to a specific effect
- a highly competitive athlete who is primarily involved in overhead or throwing sports
These patients may need to exist treated operatively because rotator cuff repair is necessary for restoration of the normal strength required to return to the preoperative, competitive level of role. Finally, those who do non answer to, or are unsatisfied with, conservative treatment should seek a surgical stance.
Surgery
The three general surgical approaches are arthroscopic, mini open, and open up-surgical repair. In the contempo past, small tears were treated arthroscopically, while larger tears would usually crave an open procedure. Advances in arthroscopy now allow arthroscopic repair of even the largest tears, and arthroscopic techniques are now required to mobilize many retracted tears. The results friction match open up surgical techniques, while permitting a more thorough evaluation of the shoulder at time of surgery, increasing the diagnostic value of the procedure, as other conditions may simultaneously cause shoulder hurting. Arthroscopic surgery also allows for shorter recovery time although significant differences in postoperative pain or pain medication utilize apparently are not seen between arthroscopic- and open-surgical patients.
Fifty-fifty for full-thickness rotator cuff tears, conservative care (i.e., nonsurgical treatment) outcomes are usually reasonably practiced. However, many patients still suffer inability and pain despite nonsurgical therapies. For massive tears of the rotator cuff, surgery has shown durable outcomes on 10-twelvemonth follow-upward. Nevertheless, the same study demonstrated ongoing and progressive fatty atrophy and repeat tears of the rotator gage. MRI evidence of fatty cloudburst in the rotator gage prior to surgery is predicative of a poor surgical effect. If the rotator cuff is completely torn, surgery is normally required to reattach the tendon to the bone.
If a pregnant bone spur is nowadays, any of the approaches may include an acromioplasty, a subacromial decompression, as office of the procedure.Subacromial decompression, removal of a small-scale portion of the acromion that overlies the rotator cuff, aims to relieve pressure on the rotator gage in sure conditions and promote healing and recovery. Although subacromial decompression may exist beneficial in the management of partial and total-thickness tear repair, it does not repair the tear itself and arthroscopic decompression has more recently been combined with "mini-open" repair of the rotator cuff, allowing for the repair of the cuff without disruption of the deltoid origin. The results of decompression alone tend to degrade with time, only the combination of repair and decompression appears to be more than enduring.
Repair of a complete, full-thickness tear involves tissue suture. The method currently in favor is to place an anchor in the bone at the natural attachment site, with resuture of torn tendon to the anchor. If tissue quality is poor, mesh (collagen, Artelon, or other degradable material) may be used to reinforce the repair. Repair can be performed through an open incision, over again requiring detachment of a portion of the deltoid, while a mini-open up technique approaches the tear through a deltoid-splitting approach. The latter may cause less injury to muscle and produce better results. Gimmicky techniques now use an all arthroscopic approach. Recovery tin can take as long as 3–six months, with a sling beingness worn for the first one–six weeks.
In a small minority of cases where extensive arthritis has developed, an option is shoulder joint replacement (arthroplasty).
Rehabilitation
Rehabilitation after surgery consists of three stages. First, the arm is immobilized so that the muscle can heal. 2nd, when appropriate, a therapist assists with passive exercises to regain range of move. Tertiary, the arm is gradually exercised actively, with a goal of regaining and enhancing strength.
Following arthroscopic rotator-cuff repair surgery, patients undergo rehabilitation to regain shoulder function. Orthopaedic surgeons stress that physical therapy is crucial to healing. Exercises decrease shoulder pain, strengthen the joint, and improve the arm'southward range of movement. Therapists, in conjunction with the surgeon, design workout regimens in accordance with individuals' needs and risk factors.
Traditionally, patients accept been advised to immobilize their shoulders for six weeks earlier doing rehabilitation. However, the appropriate timing and intensity of therapy are subject to debate. Regardless, virtually surgeons advocate to remain in the sling for at least six weeks. Some regime advocate early, aggressive rehab. They favor the apply of passive motion, which allows a patient to move the shoulder without physical attempt. Alternatively, some regime fence that therapy should be started later and carried out more cautiously. Theoretically, that gives tissues time to heal; though there is conflicting data regarding the benefits of early immobilization. A study of rats suggested that it improved the strength of surgical repairs, while research on rabbits produced contrary evidence. Patients, especially those recovering from large rotator cuff tears, are prone to developing new tears. Rehabbing too soon or also strenuously might increase the risk of retear or failure to heal. Withal, no inquiry has proven a link between early therapy and the incidence of re-tears. In some studies, patients who received before and more than aggressive therapy reported reduced shoulder pain, less stiffness and better range of movement. Other research has shown that accelerated rehab results in better shoulder function. Despite the findings, "no definitive consensus exists supporting a clinical deviation" betwixt the two methods of rehab.
At that place is consensus among orthopaedic surgeons and physical therapists regarding rotator cuff repair rehabilitation protocols. The timing and duration of treatments and exercises are based on biologic and biomedical factors involving the rotator gage. For approximately two to 3 week post-obit surgery, a patient experiences shoulder pain and swelling; no major therapeutic measures are instituted in this window other than oral hurting medicine and ice. All in all, those patients at chance of failure, should undergo a more than bourgeois approach to rehabilitations.
That is followed by the "proliferative" and "maturation and remodeling" phases of healing, which ensues for the post-obit vi to ten weeks. The effect of active or passive motion during any of the phases is unclear, due to conflicting information and a shortage of clinical prove. Gentle physical therapy guided motion is instituted at this stage, simply to foreclose stiffness of the shoulder; the rotator gage remains fragile. At three months after surgery, physical therapy intervention changes substantially to focus on scapular mobilization and stretching of the glenohumeral articulation. In one case full passive motion is regained (at normally most 4 to iv and a one-half months later on surgery) strengthening exercises are the focus. The strengthening focuses on the rotator cuff and the upper dorsum/scapular stabilizers. Typically at about six months later on surgery, about patients take fabricated a majority of the gains.
Due to the conflicting information near the relative benefits of rehab conducted early or afterwards, an individualized approach is necessary. The timing and nature of therapeutic activities are adjusted co-ordinate to patients' ages, the tissue integrity of their rotator cuff repairs and other factors. Special considerations are advisable for those who accept suffered multiple tears.
Our Shoulder Doctors:
How to Know if You Have a Damaged Rotator Cuff
Source: https://advancedortho.org/rotator-cuff-tear/
0 Response to "How to Know if You Have a Damaged Rotator Cuff"
Post a Comment